Referral Management Software Features

Intelligent Referral Routing
AI analyzes referral content, diagnosis codes, patient history, and provider specialties to route referrals to the most appropriate specialist. This minimizes delays, reduces referral leakage, and improves patient outcomes.
Automated Eligibility & Authorization Checks
AI can instantly verify insurance eligibility, policy coverage, and prior authorization requirements. This accelerates the referral process and reduces administrative burdens for both referring and receiving providers.
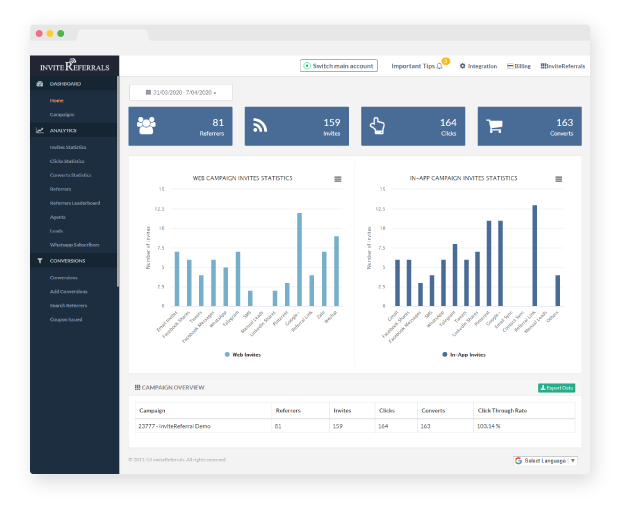
Real-Time Referral Status Tracking
AI-powered systems offer real-time visibility into referral statuses—accepted, pending, completed, or delayed—improving communication between primary care providers, specialists, and patients.
Referral Volume Prediction & Load Balancing
By analyzing historical data and provider schedules, AI predicts referral volumes and suggests optimal referral distribution across networks. This prevents overbooking and balances patient loads.
Fraud and Error Detection
AI detects patterns that may indicate duplicate, inappropriate, or fraudulent referrals by cross-referencing clinical documentation, patient records, and diagnostic justifications.
Outcome-Based Referral Optimization
AI evaluates post-referral outcomes to continuously improve referral quality. It recommends specialists based on patient feedback, treatment success, and historical effectiveness, making the referral network smarter over time.