Claims Management System Features

Automated Claims Processing & Adjudication
AI automates the review and adjudication of insurance claims by cross-checking codes, coverage rules, and medical necessity against policy data.
Real-Time Eligibility & Benefit Verification
AI tools integrated with payer databases can instantly verify a patient’s insurance eligibility, coverage limits, and preauthorization requirements.
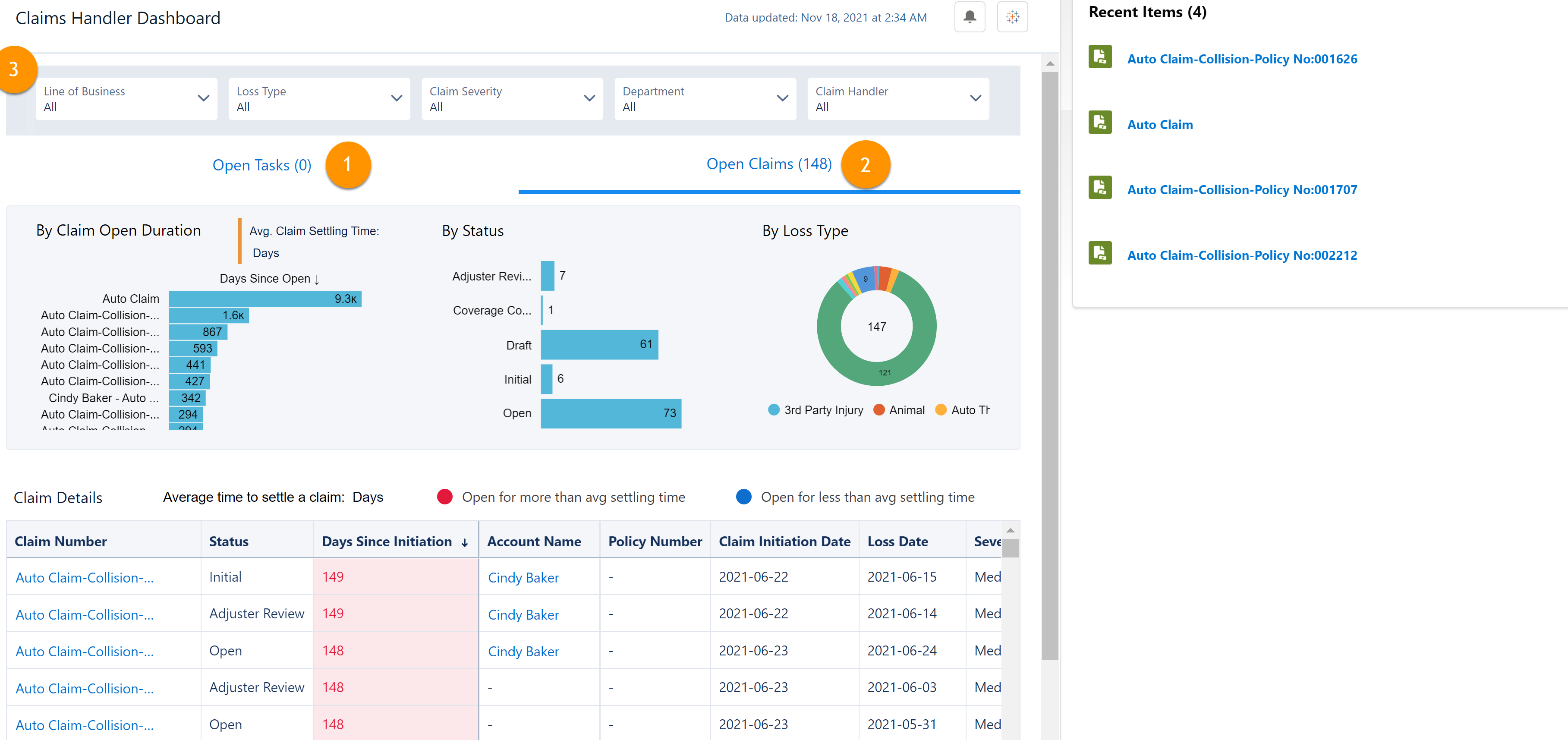
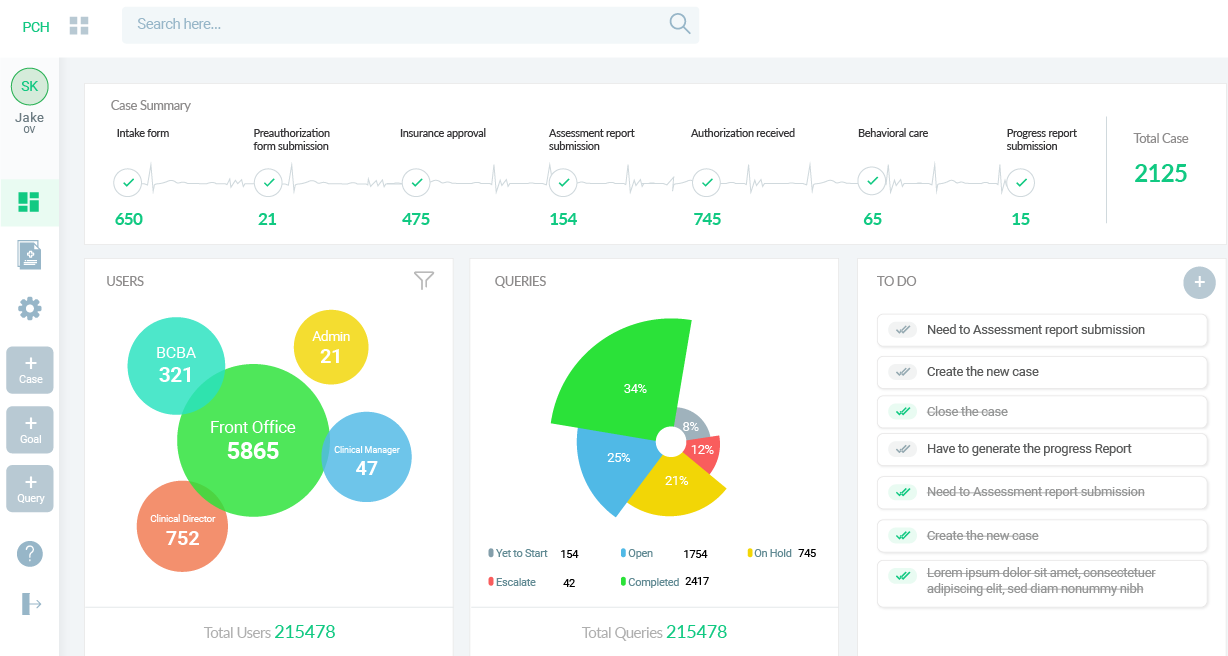
Claims Tracking
Tracks the status of submitted claims in real-time, from submission to payment.
Compliance Checks
Ensures claims adhere to legal and insurance regulations.
Fraud Detection & Risk Scoring
AI analyzes vast volumes of claims data to identify suspicious patterns, unusual billing behaviors, or potential fraud. Each claim is assigned a risk score, allowing high-risk claims to be reviewed with greater scrutiny.
Predictive Denial Management
AI analyzed historical claim denial patterns to predict which claims are at risk of rejection, offering suggestions for resubmission.